Poor sleep can lead to poor food choices
Anyone with IBS is more than familiar with the potentially rapid onset of GI symptoms after eating certain foods. Your diet is likely to be somewhat restricted, depending on your individual food triggers. However after a late-night and early-morning, have you found yourself craving certain high-calorie foods more than usual?
A group of researchers were able to demonstrate, using a functional MRI (allowing them to track brain activity), that sleep-loss significantly decreased activity in the frontal cortex and the insular cortex. These are parts of the brain that help you make “smarter” food choices.
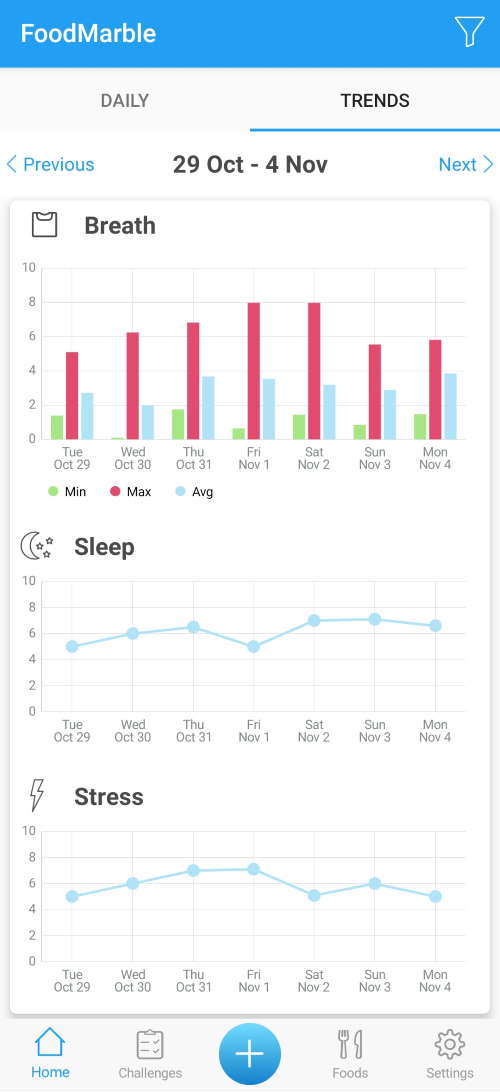
They were also able to show that activity in another part of the brain, the amygdala, was increased. The amygdala has been strongly associated with the motivation to eat. This is especially true when the salience (AKA tastiness) of the food is high. These changes appeared to be proportional to the severity of the sleep-loss. For those on the Low FODMAP diet, or following other dietary guidelines to help manage their IBS, maintaining a consistent sleep pattern can help them stick to their necessary dietary adjustments. When you track your sleep, it becomes easier to maintain a consistent sleep schedule.
Disturbed sleep, pain and reduced Quality of Life
In one study, IBS patients were compared to a group of healthy adults over a period of 7 days. During this time, their sleep patterns, pooping habits, GI symptoms and IBS-Quality of Life (QOL) were monitored. Interestingly, the IBS patients slept for more hours but felt less rested. They experienced more periods of waking up. This was a predictor of worse abdominal pain and GI distress during the following day. Also, these increased waking episodes were negatively correlated with reduced quality of life (in healthy and IBS). However, for the healthy controls there was no clear correlation between sleep disturbances, increased abdominal pain and GI distress, only a reduction in their quality of life scores.
In another study, they found a similar relationship between poor sleep quality and the occurrence of GI symptoms happening the following day. Both studies demonstrate the importance of getting some quality shut eye every night.
So, why log my sleep in the FoodMarble app?